Was sind Verwachsungen?
Bei Adhäsionen (Verwachsungen) handelt es sich um eines der am besten bewahrten Geheimnisse oder Rätsel der modernen Medizin.
Das Wort adhere bedeutet wörtlich an etwas kleben oder haften.
Wenn Gewebe, die normalerweise nicht miteinander verbunden sind zusammenwachsen, so spricht man von Adhäsion. Es wird auch den Narbengeweben zugerechnet.
Adhäsionen sind fibröse Gewebe (Narbengewebe), die Organe, die im Bauchraum liegen dazu veranlassen mit anderen Geweben, mit denen sie normalerweise nicht in Verbindung stehen, zu verkleben.
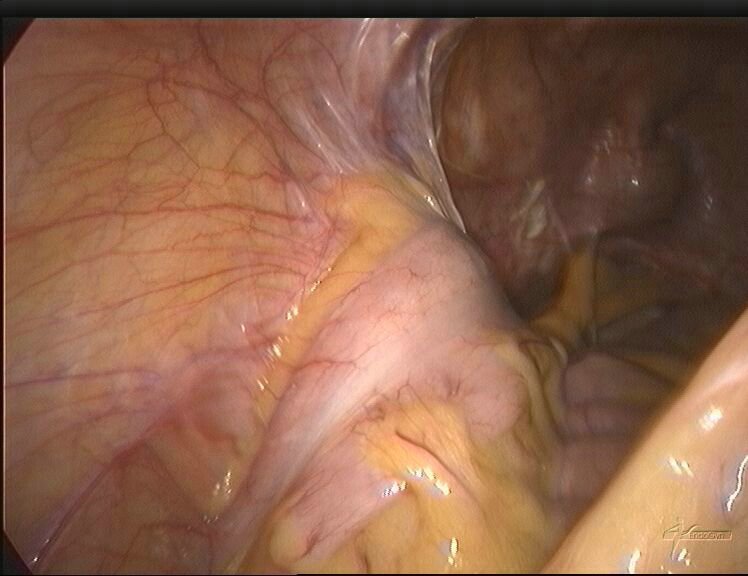
Adhäsionen können wie dünne Gewebeblätter erscheinen, ähnlich einer Plastikfolie, oder wie dicke fibröse Bänder aussehen.
Verwachsungen können die inneren weiblichen Geschlechtsorgane mit einbeziehen (Eierstöcke, Eileiter) und so Unfruchtbarkeit, Dyspareunie {schmerzhaften Geschlechtsverkehr} sowie entkräftende Beckenschmerzen verursachen.
Verwachsungen können sich überall bilden, so auch um das Herz, die Wirbelsäule und im Bereich der Hand, wo sie zu anderen Problemen führen können.
Wie verbreitet sind Verwachsungen?
Adhäsionen sind ein weit verbreitetes Problem und können im Folgenden jegliche Art von Schmerzen im Becken oder Bauch verursachen.
Die Rate von Adhäsionen nach Operationen ist erstaunlich hoch, v.a. durch das fehlende Wissen unter Ärzten und Patienten bedingt.
Adhäsionen entwickeln sich bei bis zu 93% der chirurgischen Patienten.
Diese Zahl steigt nachträglich noch an bei Patienten nach großen und mehreren Eingriffen.
Entsprechend haben einige Studien herausgefunden, dass 93% der Patienten, die mindestens eine Bauchoperation hatten, Adhäsionen aufwiesen, im Vergleich zu nur 10,4 % der Patienten, die noch nie am Bauch operiert wurden.
Die Häufigkeit von Verwachsungen stieg auch mit der steigenden Anzahl gynäkologischer Eingriffe.
Es zeigt sich, dass zwischen 60 – 90 % der Frauen, die eine große gynäkologische Operation hatten, danach unter Adhäsionen leiden.
Arten von Verwachsungen
Das Gewebe entwickelt sich, wenn Reparaturmechanismen des Körpers auf eine Gewebezerstörung wie bei Operationen, Infektionen, Trauma oder Bestrahlung reagieren.
Obwohl Verwachsungen überall auftreten können, sind die häufigsten Lokalisationen im Bauch, dem Becken sowie am Herzen.
Adhäsionen im Becken:
- Verwachsungen im Bereich des kleinen Beckens können andere Beckenorgane miteinbeziehen wie zum Beispiel die Gebärmutter, die Eierstöcke, die Eileiter oder die Blase, und treten häufig nach Operationen auf.
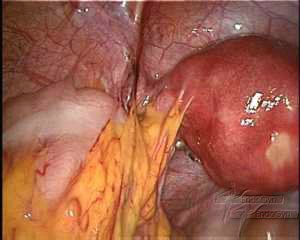
Adhäsionen zur vorderen Gebärmutterwand

Adhäsionen zwischen Gebärmutter, Adnexen und Eingeweide
- Entzündliche Erkrankungen im Becken (PID) resultieren aus einer abgelaufenen Infektion, (häufig eine sexuell übertragene Krankheit) die oft zu Adhäsionen im Bereich der Eileiter führt.
- Eine reife Eizelle passiert die Eileiter zur Gebärmutter während des Eisprungs.
- Eileiteradhäsionen können zu Unfruchtbarkeit führen und erhöhen das Risiko einer extrauterinen Schwangerschaft, die sich in den Eileitern entwickeln kann.
Verwachsungen im Bauchraum:
- Abdominelle Verwachsungen sind im Allgemeinen Komplikationen einer Operation, die bei bis zu 93 % der Patienten auftreten, die sich einer Bauch- oder Beckenoperation unterzogen haben.
- Abdominelle Adhäsionen treten auch bei 10,4 % der Personen auf, die nie operiert wurden.
- Die meisten Verwachsungen verursachen keine Schmerzen oder Komplikationen.
- Jedoch, in ca. 60-70 % verursachen Verwachsungen kleine Obstruktionen im Bereich der Eingeweide und tragen wahrscheinlich zur Entwicklung chronischer Beckenbeschwerden bei.
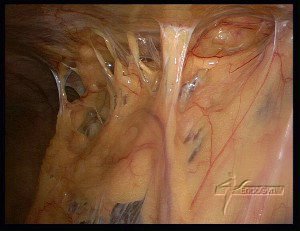
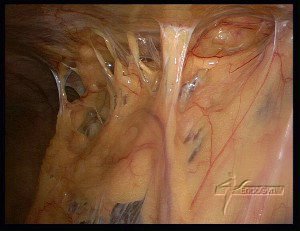
Darmverwachsungen

- Verwachsungen bilden sich typischerweise in den ersten Tagen nach einer Operation, aber es ist möglich, dass sie zunächst für Monate oder Jahre keine Symptome verursachen.
- Wenn das Narbegewebe beginnt die Bewegungsmöglichkeiten der Intestinalorgane einzuschränken wird der Transport von Nahrungsmitteln durch den Darmtrakt zunehmend schwieriger.
- Es kann zu einem Passagestopp kommen (Darmverschluss).
- In Extremsituationen bilden die Adhäsionen fibröse Bänder um einen bestimmten Darmabschnitt herum. Dabei wird dann der Blutfluss abgetrennt und das Gewebe stirbt ab.
„De novo“ Adhäsionen
- Bei „de novo“ Verwachsungen handelt es sich um neu aufgetretene Adhäsionen, die sich an der Stelle eines direkten chirurgischen Traumas bilden wie bei einem chirurgischen Schnitt.
- Sie können sich auch an Stellen bilden, die von dem ursprünglichen Operationsort entfernt liegen.
- Verwachsungen können sich auch nach Adhäsiolyse oder Adhäsionstrennung neu bilden.
Es existieren drei Haupttypen von Verwachsungen, wobei der zugrundeliegende Pathomechanismus sich ähnelt:
- Hauchdünne
- Vaskularisierte (Gefäße beinhaltend)
- Zusammenklebende
Verwachsungen sind Komplikationen von Operationen !
Gepostet am Mrz 16, 2010 in Verwachsungen
Lassen Sie es nicht zu, dass bei Ihnen Verwachsungen entstehen !
Möglichkeiten, um die schmerzhaften und gefährlichen Folgen zu verhindern, unter denen bis zu 93% der Patienten nach Bauchoperationen zu leiden haben.
Gesetzt der Fall, bei 9 von 10 Patienten würden postoperative Infektionen entstehen, würde da der Arzt nicht Antibiotika oder ihre Dosierung ändern?
Natürlich würde er das tun !
Deshalb ist es erstaunlich, dass nicht mehr getan wird, um Verwachsungen zu vermeiden, die doch bei bis zu 93 Prozent der Patienten nach Bauchoperationen und nach Unterleibsoperationen entstehen. Ärzte schweigen während die Patienten leiden…
Verwachsungen:
meist nach Operationen bilden sich dünne Gewebestränge und haften an inneren Organen, die normalerweise nicht miteinander verbunden sind. Dies geschieht nach jeder Operation, egal ob es sich um eine Laparoskopie (Bauchspiegelung) oder eine Laparotomie (Bauchschnitt) handelt.
Aber es ist in Zukunft nicht nötig, dass Sie und andere Patienten unter Verwachsungen und deren schmerzhaften Folgen leiden. Es gibt Operationstechniken und spezielle Verwachsungen Barrieren, um Verwachsungen zu vermeiden.
Verwachsungen sehen manchmal aus wie dünne Plastikfolien oder auch wie dicke Gewebestränge. Sie können zu Darmverschlüssen und Notoperationen führen und manchmal auch tödlich enden. Sehr häufig führen Verwachsungen zu chronischen Schmerzen und bei Frauen zu Unfruchtbarkeit, falls Verwachsungen sich an den weiblichen Fortpflanzungsorganen festgesetzt haben. Dies sind nur einige Beispiele.
Sie mindern die Lebensqualität der Patienten, führen oft zum Verlust von Arbeitsplätzen oder Berentungen, tragen zum Verlust von Produktivität und erhöhen das Risiko von schweren Komplikationen bei nachfolgenden Operationen. Darüber hinaus ist bei Patienten, die weitere Operationen vornehmen lassen müssen nicht nur das Risiko höher, dass sich noch mehr Verwachsungen bilden, sondern es ist, wie Studien gezeigt haben, bei 19-33% der Patienten der Fall, dass sie während dieser Operationen verwachsungsbedingte Darmperforationen (Verletzung des Darmes) erleiden. Dies führt wiederum zu bedeutend höheren Risiken: Bauchfellentzündung, längerer Krankenhausaufenthalt und postoperativer Komplikationen wie zum Beispiel Blutungen und Wundinfektionen.
Kurzum, es ist ein Teufelskreis und die Patienten sind mit dem Problem der Verwachsungen meisten allein gelassen. Es ist schwierig, dies zu vermeiden, denn Verwachsungen können praktisch nach jeder gynäkologischen Prozedur, Unterleibsoperation oder anderen Operationen im Bauch entstehen, einschließlich Eierstocksoperationen, Operationen zur Entfernung von Endometriose, Myomentfernungen, Gebärmutterentfernungen, Eileiterrekonstruierung, Darmoperationen, Bruchoperationen, Gallenblasenoperationen, Verwachsungs-Operationen, Verwachsunglösungen bei Darmverschlüssen, Blinddarmoperationen, Krebsoperationen, und Leber-und Milzoperationenen.
Es gibt verschiedene Faktoren, die zu Verwachsungen führen:
Trauma
Operationen stellen ein Trauma dar und der Körper produziert Verwachsungen als Verteidigung gegen dieses Trauma als normaler Beitrag zum Heilungsprozess.
Reduzierung der Gewebedurchblutung (Ischämie)
Während einer Operation kann das Durchschneiden von Gewebe, die Entstehung von Blutgerinnseln oder das Vernähen der Wunde die Durchblutung behindern, so dass eine Ischämie entsteht, was die Entstehung von Verwachsungen begünstigt.
Fremdkörper
Fäden, Flusen von Tüchern und Puder von Operationshandschuhen gehören zu den Dingen, die den Weg in den Körper des Patienten finden und Entzündungen verursachen können, was wiederum zu Verwachsungen führt.
Entzündungen
Endometriose und Unterleibsentzündungen können ebenfalls zur Verwachsungsbildung führen.
Wie häufig sind Verwachsungen?
Studien haben ergeben, dass sich bei 93% aller Patienten nach einer Bauchoperation Verwachsungen gebildet haben. Dieser Prozentsatz ist noch höher bei Patienten mit mehreren oder komplizierten Operationen.
Studien haben weiterhin ergeben, dass nur bei 10,4% aller Patienten, die nie eine Operation hatten Verwachsungen entstanden sind.
Die Wahrscheinlichkeit dass Verwachsungen bei Frauen entstehen wird höher, je mehr gynäkologische Operationen durchgeführt werden. Man hat festgestellt, dass zwischen 60 und 90% aller Frauen nach diesen Operationen an Verwachsungen leiden.
Verwachsungen sind verantwortlich für
49 bis 74% Dünndarmverschlüsse
15 bis 20% Unfruchtbarkeit und
20 bis 50% Chronische Unterleibsschmerzen
Verschiedene Methoden, aber keine Garantie
Obwohl es nicht möglich ist, das Verwachsungsrisiko gänzlich zu vermeiden, können Ärzte verschiedene Schritte vornehmen, die die Wahrscheinlichkeit der Verwachsungsbildung verringern. Die effektivste Methode schließt eine optimale Operationstechnik ein und die Anwendung einer physikalischen Barriere, um die Gewebeoberflächen während des Heilungsprozesses getrennt zu halten.
Eine gute Operationstechnik ist der erste Schritt und beinhaltet diese Schritte:
Stoppen von Blutungen
Ist dies unzulänglich, sind die Folgen Fibrinablagerungen, was wiederum Verwachsungen begünstigt. Das Vermeiden und rechtzeitige Stoppen von Blutungen und somit von Fibrinablagerungen ist also von äußerster Wichtigkeit.
Das Befeuchten von Gewebe
Das Gewebe muss stets feucht gehalten werden durch das Benutzen von feuchten Tüchern, um ein Austrocknen des Gewebes zu vermeiden. Ringerlaktat oder andere Feuchtigkeitslösungen verhindern auch, dass Talkumablagerungen oder Blutgerinnsel einen Krankheitsherd schaffen, auf den der Körper reagiert mit Entzündungen und Verwachsungen.
Trockene Tücher vermeiden
Verwenden sollten Ärzte keine trockene (Mullbinden und -tücher, da diese das Bauchfellgewebe stören und einen Fremdkörper hinterlassen können.
Feine und atraumatische Nähte
Die feinsten Nähte und Fäden aus synthetischem, nicht reagierendem Material vermindern Fremdkörperreaktionen.
Das Gewebe so wenig wie möglich berühren
Wenn das Gewebe zu sehr manipuliert wird, ist die Wahrscheinlichkeit groß, dass Schäden an Gewebe und Blutgefässen entstehen. Wenn es wirklich notwendig ist, das Bauchfell direkt zu manipulieren, so sollten immer atraumatische Instrumente eingesetzt werden.
Bauchschnitte und Blutungen müssen möglichst vermieden werden
Am besten eignet sich die weiter unten vorgestellte endoskopische Operation mittels der gaslosen Lift-Bauchspiegelung (gaslose Lift-Laparoskiopie). Sie vermindert Trauma und Blutverlust und in Verbindung mit den obengenannten Techniken bietet sie die beste Möglichkeit das Entstehen von Verwachsungen zu reduzieren.
Vermeiden von Fremdkörpern
Sie können die Bauchfelloberfläche beschädigen, zu Entzündungen führen und letzendlich Verwachsungen verursachen.
Verschiedene Medikamente, die gewebelösende Inhaltsstoffe enthalten, Antikoagulantien, Entzündungshemmer und Antibiotika wurden ausgewertet, in dem Bemühen, Verwachsungen zu reduzieren. Bis zum heutigen Tag hat keine noch so gut kontrollierte Studie die Effizienz dieser Medikamente belegen können. Das mechanische Trennen von Gewebe ist auch eine Möglichkeit und das Einsetzen von Barrieren zwischen Wundgewebeoberflächen scheint eine der vielversprechenden Methoden zur Vermeidung von Verwachsungen zu sein. Jedoch hat sich noch keine der gegenwärtig eingesetzten Barrieremittel und endogenen Netze, die in den Bauchraum eingebracht werden in verschiedenen Studien als effektiv erwiesen.
Vielversprechend
Dr Kruschinski’s Techniken zur Operation und Vermeidung von Verwachsungen:
„Die Methode, die ich im Kampf gegen Verwachsungen als die wirkungsvollste erachte, ist die gaslose Lift-Laparoskopie mit dem Abdo-Lift. Hierbei wird zum Anheben der Bauchdecke ein Lift-System eingesetzt, anstatt des Aufblasens mit dem Kohlendioxid-Gas bei der üblichen Bauchspiegelung. Das Kohlendioxid wird nämlich im Bauchfell zur Kohlensäure umgewandelt, so dass das Bauchfell und Organe angesäuert werden und niedrige pH-Werte entstehen, die zum Zelltod führen, was zusätzliche (neben dem Operationstrauma) Verwachsungen verursacht. Weiterhin entzieht das Kohlendioxid dem Gewebe Sauerstoff, wodurch eine sog. Hypoxämie (Sauerstoffmangel) des Gewebes entsteht, was wiederum zum Zelltod und Verwachsungen führt. Deshalb hat, laut Studien, die Methode der üblichen Laparoskopie mit CO2-Gas zu KEINER Senkung der Re-Operationen wegen Verwachsungen geführt“
Neben dieser Operationstechnik setzt Dr. Kruschinski aber auch spezielle Verwachsungen-Barrieren ein, wie z.B. das SprayShield™, welches zur Vorbeugung von Verwachsungen führt. Dieses Gel wird auf die Wundflächen, die bei der Operation entstehen, aufgesprüht, haftet dort für ca.7 Tage und wird dann resorbiert und über die Niere ausgeschieden, also verschwindet vollkommen aus dem Körper, nachdem es seine Aufgabe, die Wundfläche vor Verklebungen (Verwachsungen) zu schützen, erledigt hat. Es kann alleine oder bei größeren Wundflächen in Kombination mit anderen Barrieren, wie etwa Adept®, eingesetzt werden.
„Da sich Verwachsungen schon ab 3 Stunden nach Ende des Operationsvorganges bilden können und sich weiter entwickeln bis zu 72 Stunden nach dem Eingriff, führe ich eine second look Laparoskopie am 5-7.Tag bei Verwachsungs-Patienten durch. Falls ich sehe, dass sich wieder Verwachsungen angelegt haben, können diese „unblutig“ mit Hilfe von Wasser (Aquadissection) leicht entfernt werden. Ich habe dieses Vorgehen bereits an mehreren hundert Patienten durchgeführt und es reduziert in hohem Masse die Notwendigkeit einer Folgeoperation. In meinem Patientenkollektiv sind ca. 85% der Patienten verwachsungsfrei in dieser zweiten Laparoskopie. Das bedeutet, dass nur 15% Schmerzen haben oder sie nach der Operation wieder entwickeln und mussten sich noch einer sog. third-look Laparoskopie unterziehen. In der Hälfte dieser Fälle waren Verwachsungen die Ursache der Schmerzen, es gab aber auch andere Gründe für die Beschwerden wie zum Beispiel Eierstockszysten oder Endometriose. Insgesamt waren die Verwachsungen aber auch in dieser Gruppe niedriger im Score, wenn man Grad und Ausmaß der Adhäsionen vergleicht mi der ersten Operation vergleicht. Somit waren diese third-look-Verwachsungsoperationen weniger extensiv und es musste weitaus weniger Gewebe geschnitten werden als in den vorherigen Operationen.“
Packen wir das Problem an
Verwachsungen können unglaublich schmerzhaft sein und führen dazu, dass die Patienten einen Arzt nach dem anderen aufsuchen, um davon geheilt zu werden. Sich einer Operation zu unterziehen, birgt viele Risiken gefahren. Viele Patienten werden zudem durch diese Bauchschnitte entstellt und verunstaltet, die wieder Verwachsungen verursachen. Die Ärzte wissen immer mehr und lernen immer mehr darüber wie man Verwachsungen bekämpfen kann. Diejenigen Ärzte, die nicht über Verwachsungen und deren Behandlungsmöglichkeiten aufklären, vernachlässigen ihre ärztlichen Pflichten. Es sollte möglichst alles dafür getan werden, dass bei Patienten Bauchschnitt-Operationen vermieden werden, was heute in 99 % der gutartigen Befunde möglich ist. Bei bereits vorhandenen Verwachsungen, sollten diese Patienten an spezialisierte Zentren mit einer Infrastruktur, wie oben beschrieben, überwiesen werden.
Auswirkungen von Verwachsungen
Die Auswirkungen von Adhäsionen auf den Patienten:
- Verwachsungen sind für 49- 74 % der Darmverschlüsse im Dünndarm verantwortlich.
- Verwachsungen verursachen 15- 20 % der Unfruchtbarkeitsfälle.
- Adhäsionen verursachen 20- 50 % der Fälle chronischer Beckenschmerzen.
- Reduktion der Lebensqualität.
- Verwachsungen verursachen Krankheitstage und einen Verlust der Produktivität
- Die Folgeoperationen sind komplexer und mit einem immens erhöhten Risiko von Komplikationen.
- Eine Studie zeigt eine Rate von 19 % adhäsionsbedingter Darmverletzungen bei folgenden oder Zweitoperationen.
- Patienten mit adhäsionsbedingten Eingeweideperforationen hatten postoperativ eine deutlich höhere Komplikationsrate (Lecke, Wundinfektionen, Blutgerinnungsstörungen und einen längeren Krankenhausaufenthalt)
Die Auswirkungen von Adhäsionen auf Chirurgen:
- Längere Operationszeiten
- Erhöhtes Risiko einer Darmverletzung
- Ein erhöhtes Niveau der chirurgischen Komplexizität
Verwachsungen: ein Dilemma !

Bei 93 % aller Bauchschnitte entstehen Verwachsungen.
Von 100 Operationen werden 10 im ersten Jahr wieder aufgenommen,
d.h. ein 10 % Risiko, das Sie nach einem Bauchschnitt wegen Verwachsungen wieder aufgenommen werden müssen
Daten aus der Scar – Studie
***************************
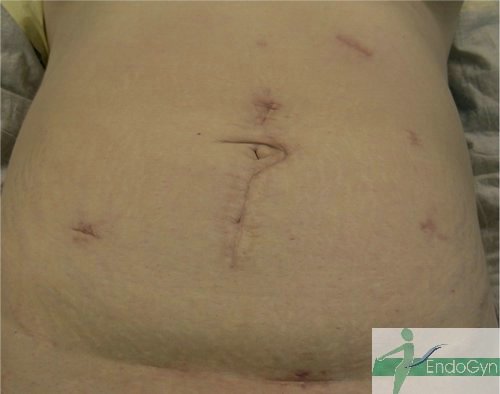
Schauen Sie sich an, wie Menschen durch vermeidbare Bauchschnitte verunstaltet werden.
Vermeiden Sie unter allen Umständen einen Bauchschnitt !
Bei 99 % aller gutartigen Erkrankungen ist in unserer Hand eine endoskopische Operation möglich.
www.Bauchschnitt-Nein-Danke.de

















Eine seltene, aber schlimme Komplikation ist eine eitrige Infektion der Bauchschnittnarbe, die eine offene sog „Sekundärheilung“ erfordert. Die Wunde wird dabei offen gelassen und täglich gesäubert und desinfiziert, bis sich diese irgendwann mal dann langsam und mühsam von unten von selber schliesst.


Nach einer Langzeitstudie leiden 5% aller per Bauchschnitt operierten Patienten später unter Darmverschlüssen [1]
Postoperative Verwachsungen sind die vorherrschende Ursache für einen Darmverschluss in der westlichen Welt. [2]; hierbei ist die Tendenz steigend.
Die SCAR-2 Studie (1) an gynäkologische Eingriffe per Bauchschnitt und per Bauchspiegelung mit Gas zeigte 35% Wiederaufnahmen wegen Verwachsungen in den ersten 4 Jahren nach Operation.
Somit senkt auch eine Operation mittels einer Bauchspiegelung mit CO2 Gas das Risiko für Verwachsungen nicht.
Britische Studien aus den Jahren 1985/1986 belegen, dass mittlerweile schon für etwa 32% der Darmverschlüsse die Verwachsungen verantwortlich sind [3].
In den Fällen von Dünndarmverschlüssen seien in 60 – 70 % Verwachsungen beteiligt (4).
Treuter beschreibt, dass heute 76% der Fälle von mechanischem Dünndarmverschluss durch Adhäsionen bedingt sind.[5]
1 Lower AM, Hawthorn RJ, Clark D, et al (2004) Adhesion-related readmissions following gynaecological laparoscopy or laparotomy in Scotland: an epidemiological study of 24 046 patients. Hum Reprod 19:1877–1885
2 Ellis H.: Prevention and treatment of adhesions.. Infect Surg. 1983, 11, S.803-807,
3 McEntee G.: Current spectrum of intestinal obstruction.. Br J Surg. 1987, 74, S.976-980,
4 Ellis H.: The clinical significance of adhesions: focus on intestinal obstruction.
Eur J Surg Suppl. 1997;(577):5-9. Review.
5 Treutner K.-H.: Prophylaxe und Therapie intraabdomineller Adhäsionen: eine Studie an 1200 Kliniken in Deutschland Der Chirurg 1995, 66, 398-403
Abgesehen von Komplikationsmöglichkeiten, wie offene Wunden, hässliche Narben etc. gehen Sie also, wenn Sie einen Bauchschnitt akzeptieren, ein 5%-ges Risiko ein, einen Darmverschluss zu bekommen!
Ein Darmverschluss ist eine lebensgefährliche Komplikation von Verwachsungen und somit bedeutet ein Bauchschnitt potentiell das Risiko, sich in 5% in Lebensgefahr zu bringen.
Vermeiden Sie deshalb unter allen Umständen einen Bauchschnitt und dessen gefährliche Komplikationen !
Bei 99 % aller gutartigen Erkrankungen in der Gynäkologie ist in unserer Hand mit Hilfe der modernen und schonenden Lift-Laparoskopie (Bauchspiegelung OHNE Kohlendioxidgas) eine endoskopische Operation OHNE Bauchschnitt möglich.
Lassen Sie sich durch Ihre/n Ärztin / Arzt in dieser Praxis beraten und besuchen Sie unsere Seiten im Internet.
Ezine Artikel
|
Articles taken from www.ezinearticles.com Adhesions – What a Pain!Woe to the woman who suffers in illness, unrelenting illness. Though medicine and science has made great strides in the battle against many illnesses, there is an illness that is hushed; shrouded in silence among many physicians. Far from being rare, this illness carries with it staggering statistics, yet the public at large is not privy to this-often debilitating-disorder: adhesions. Adhesions, the body’s natural response to infection, inflammation or injury, are bands of scar tissue that can form inside the body causing the internal organs to fuse together. *Over 93% of patients who undergo major abdominal or pelvic surgery will develop adhesions. Adhesions, quite common, are known to form in as many as 60 to more than 90% of women undergoing gynecologic surgery. In the medical world, adhesions are foremost known to be an iatrogenic disorder-meaning caused by the physician or by medical treatment (or both)-yet prior to surgery, the surgeon rarely informs his patient of the risk of developing adhesions. For the fortunate person who is not scheduled for surgery, the risk of adhesions is still a concern. Adhesions can develop as a result of infection or an inflammatory condition. Endometriosis, PID (pelvic inflammatory disease), appendicitis, peritonitis, trauma to the body (including surgical trauma), and even radiation, are all examples of health conditions or treatments that produce favorable conditions for the development of adhesions. *Adhesions were first documented in 1872…..yes, 1872, yet most people, when asked, have never heard of adhesions. Thomas Bryant made that first documentation when he reported a fatality due to adhesion-related bowel obstruction after gynecologic surgery. Over the next 130 years, adhesions have maintained prominence in the medical literature, both as a study topic and as a factor influencing various treatments and outcomes. Though adhesions have maintained prominence in medical literature as a study topic and a factor that influences various treatments and outcomes, adhesions have, for the most part, remained hidden to the public at large. The doctors may be studying, but they’re sure not talking-at least not to their patients. When a person is suffering from the dreaded disorder, adhesions, it is likely the last thing on the list that a doctor will mention as a plausible cause of the pain and problems that are going on within the body. And, more often than not, the condition will never be mentioned at all, although the person may be presenting with all the symptoms of adhesions, or adhesion related disorder. Of course, this sends the sufferer roaming the beautiful globe in search of a doctor who gives a big rat’s whisker about their condition. On the average, a woman will suffer 7-10 years, going in and out of doctors‘ offices in search of an answer to their pain and symptoms. Adding insult to injury is the fact that adhesions elude the probing eye of standard medical tests, such as X-rays, scans, MRI’s, etc. Diagnostic laparoscopy (minimally invasive surgery) is the only means by which to properly diagnose adhesions. How can you determine if you might be suffering from adhesions? Adhesion sufferers describe their pain as intense, stabbing, sharp, and/or pulling. Some sufferers cannot walk uprightly, as adhesions restrict mobility. Simple movement such as bending and stretching can be compromised. Many sufferers experience frequent nausea, which often leads to vomiting. Many sufferers state that they feel „worse“ after eating a meal-though they were hungry-often lamenting having eaten at all. When the intestines are involved with adhesions, a bowel obstruction can occur. A bowel obstruction is described as intense abdominal pain, nausea, and often, vomiting. A bowel obstruction is a life-threatening emergency, requiring immediate medical care. (Keep in mind that others may experience different symptoms than those that are described here.) In addition: though this article is geared toward women, men can also suffer from adhesions. Trauma to the body (a blow to the abdomen, for instance) surgery, or even a seat belt injury, can cause intestinal adhesions in men. For the adhesion sufferer, it is time for knowledge of this disorder to be at the forefront of medicine. For the doctor and surgeon, it is time to talk-to your patient. Sources: *Confluent Surgical *Bryant T. Clinical lectures on intestinal obstruction. Med Tim Gaz 1872;1:363-5.
Adhesions – After the Fact
At some point in life we have all experienced the „why didn’t you tell me?“ scenario. Whether we’ve just downed a bowl of homemade potato salad, enjoying every last bite, only to have the best potato salad maker in the world walk into the kitchen–a look of horror on her face–and state: „I left that on the counter because I intended to throw it out! Don’t tell me you just ate it!“ (Well, of course we ate it. Isn’t that how it always goes?) „Why?“ the satisfied, but now worried eater asks, „don’t tell me it is spoiled!“ „Well, no it’s not spoiled,“ the cook answers nervously, „well, yes, I guess it is spoiled…okay..yes, it is spoiled.“ „Well, great! That’s just great! You leave it on the counter all day and then I come in, thinking you just made it, and now you’re telling me that I’m going to die from that weird salmon poisoning?“ „Salmonella. And for your information, I did just make it…I didn’t leave it on the counter all day. And even better news: I don’t think you’ll die.“ The eater stares at the cook. „Okay, so tell me! What’s the deal with the potato salad?“ „No deal. It’s just that…well, you know that overgrown dog of yours? The four-legged hairy creature that you just adore? The one you call Outlaw? The one I despise because he has no manners?“ „Don’t tell me…“ „Yep; he loves potato salad just as much as you.“ In that moment, we gag…for we have gained knowledge after the fact. Oh how we wish we had only known. In moments like these, when one person has knowledge that another person does not have, we realize our vulnerability. In the above scenario, the cook can’t really be blamed. She had good intentions. She intended to dump the potato salad. So, we realize we need to forgive, even though we gag. But, what if the cook had ill intentions? Or, what if she just didn’t care, so she withheld information? What if she knew the dog wolfed down half the potato salad, but she allowed her boyfriend to come in, eat what was left, yet never uttered a word to him? We might call her a cold, calloused miscreant. We all know that anyone who cares about another human being is going to say: „Don’t eat the potato salad! The dog got into it!“ Today, there are major surgical procedures being performed and, more often than not, women are not being informed of the high risk of future health issues that might arise due to these procedures. C-section procedures have become all the norm in the USA, with the National Center for Health Statistics reporting a preliminary US national cesarean rate of 31.1% in 2006. In times past, a c-section was only performed if the life of the mother or baby, or both, were at stake. Today, however, c-sections as an elective procedure seem only to be rising. More and more women, most often at the urging of their doctor, are scheduling surgery as a means by which to bring their unborn child into the world. Though many doctors are pushing c-sections births, these same doctors are not informing their patient that a c-section is not only major abdominal surgery, (risky; as well as a much longer recovery time, while trying to care for the new baby) but that a laparotomy (open abdominal incision) puts a woman at a high risk for developing adhesions. Adhesions (scar tissue that forms as a result of the incision) can cause internal organs to become fused together. *In fact, 93% of patients undergoing major abdominal surgery will develop adhesions, with 53% of those people developing (at some point in their lives) a problematic condition known as adhesion related disorder (ARD). If women only knew that the c-section they schedule today might result into a condition that can be a life-altering and debilitating disorder later, they might very well insist that their baby be born the old-fashioned way: vaginal birth. The patient (and all mother’s-to-be) should be informed patients. The patient should be allowed the chance to weigh the benefit of surgery against the risk of developing a debilitating disorder. Unfortunately, many women who are now suffering the devastating effects of Adhesion Related Disorder learned about adhesions after the fact. Since doctors and surgeons are keenly aware that open abdominal surgery creates scar tissue (adhesions), it is reprehensible that any woman become the victim of adhesion related disorder as an after the fact illness. Source: *EndoGyn
©Karen Steward
Crohn’s Disease and Adhesions – Diagnosing Disease If you have never experienced a bowel obstruction, count yourself blessed. For years I watched my daughter suffer in intense, incredible, (at times, screaming) pain, yet she was ignored by countless physicians. These physicians never once stated that she was suffering from a bowel obstruction -rather, we (her parents) were told she must LIVE with the pain and agony of Crohn’s disease. The solution to her misery was always the same: up her steroid. Little did it matter that she spent days, weeks, sometimes months on end, hovering over the toilet….begging God to help her, crying in pain. The same physicians used simple terminology for these agonizing episodes: narrowed bowels. They showed us x-rays to prove their theory. And yes, we could see the bowel had many areas that were narrowed – portions of the bowel appearing to have a string-like appearance. I always had the same question: Does my daughter truly have Crohn’s? Based on studies I had done, I doubted the diagnosis; thus we spent years roaming the USA in search of an answer that I could believe. Along the way, I learned that she was suffering from bowel obstructions, brought on by these „narrowed bowels.“ Perseverance paid off, and paid off big. Today, my daughter is well. We now know that she was suffering from adhesions. Those „narrowed bowels“ were actually adhesions (scar tissue) that were encased around her large and small bowel, strangling the bowel to the point of little function, while leaving her in debilitating pain. The surgeon in Europe who was able to restore our daughter’s health said he saw no sign of Crohn’s disease. Though we may never know the true culprit behind our daughter’s illness, we speculate that the adhesions were the result of an infection or inflammation in the body. Since she had suffered from ovarian cysts at the beginning of her menses, it is likely that scar tissue began forming as a result. Since bowel obstructions (caused by formation of adhesions) are the most common complication in Crohn’s disease, it is easy for the physician to sum up a patient as a Crohn’s sufferer when x-rays reveal „narrowed bowels.“ For the person who is incorrectly labeled with Crohn’s disease, the road to a correct diagnosis, as well as recovery of illness, is one that is treacherous indeed. The payoff, however, can be worth every ounce of required effort.
Adhesions and ARD Awareness – It’s No Hoax!For the many people who suffer from abdominal adhesions or have lost years of their life due to this medical malady, the recent Internet hoax about Subway spokesman, Jared Fogel’s death (due to abdominal adhesions), is less than humorous. However, since it is best to look on the bright side of life, perhaps Jared’s faked death will help bring awareness to the plight and very dismal world of the adhesion sufferer. (As a token of thanks, I’m hoping Jared will write me so I can send him an ARD awareness pin!) Adhesions are known to develop in 93% of people who undergo major abdominal or pelvic surgery with 53% of those people developing health related complications at some point in their lives due to adhesion formation. Adhesions can cause the internal organs to become fused together, leaving the victim to suffer incredible–often agonizing–pain, while searching in vain for a doctor who will diagnose the correct ailment that is going on in his or her body. On the average, a person will suffer 7-10 years before learning that they are actually suffering from adhesion formation. And yes, gastric bypass surgery, as any surgery, can result in adhesion formation that can be severe, even life-altering, in some cases. Adhesion sufferers lives are often swallowed up–lost in a world of pain–which costs them everything: jobs, friends and often, even family. Adding insult to injury is the fact that adhesions elude the eye of standard medical tests (x-rays, scans, MRI’s, etc), leaving many doctors to misdiagnose a patient or, worse yet, diagnose those who suffer as ‚depressed‘ individuals; totally ignoring the fact that the patient’s pain is REAL. Adhesions, foremost known among the medical world as an iatrogenic disorder, is an illness that is a hot topic among physicians but one that is often shrouded in silence when a doctor meets with a patient who presents with all the „symptoms“ of adhesion related disorder. Simply put: most doctors do not want to deal with an adhesion sufferer, thus a diagnosis of „depression“ can also be a ploy by which the physician can be assured that he (she) has washed his (her) hands of this problematic patient (condition). For the adhesion sufferer, perhaps the only thing more devastating than living in horrid pain is meeting the many physicians whose quick analysis of her (his) condition is: psychosomatic illness. Unfortunately for the adhesion sufferer, the written prescription for an antidepressant can be used to the physician’s advantage. That insulting piece of paper-„depression discharge slip“- frees the doctor from the dread ailment/patient–and is an effective means to push the adhesion sufferer out the door and on to the next doctor who will likely follow the same course of action. For the adhesion sufferer, a „diagnosis“ of depression and a quickly scribbled RX for an antidepressant is a heartwrenching and emotional low blow for the person who is merely existing in a body that is entrapped by pain. The depression discharge paper sets in motion the tiresome and weary journey of going from one doctor to the next; thus years of quality life are lost to adhesion related disorder (ARD).
Adhesions – The Uphill JourneyThe Little Pain That Could – An Uphill Journey Toward Adhesion Awareness I think I can. I think I can. I think I can. Sadly, much as we’d like to believe otherwise, some obstacles can’t be overcome by willpower alone. That pain in your belly won’t go away simply because you’re being brave and doing your best not to let it overtake your life. In fact, you don’t feel at all like a courageous little engine when your doctor tells you it’s just „all in your head.“ Clearly the pain is quite a bit lower than your head, but when all the tests come back normal, a tiny piece of you may wonder whether you really should give up and just deal with it. But what would the Little Blue Engine do in your circumstances? The savvy little locomotive would consider alternatives! You know your pain isn’t IBS because you’ve already gone through the treatments and they haven’t helped. Neither have the treatments for Crohn’s disease, spastic colon and bowel obstructions. Could the pain you’re feeling be adhesions? Adhesions, otherwise known as scar tissue, are fibrous bands that form at the site of injury. The scar tissue can fuse internal organs together, pulling them away from their normal positions. This causes loss of flexibility by preventing the intended and natural fluid movement of the organs and results in excruciating and often debilitating pain. Since surgery is injury (trauma) to the body, adhesions can form at the site of the incision. Adhesions also can form in the body as a result of infection or inflammation such as appendicitis, peritonitis, sexually transmitted disease and radiation. Because adhesions do not show up on standard medical tests such as X-rays, scans, and MRI’s, the condition is often misdiagnosed. Adhesion sufferers spend an average of 7-10 years before they find an answer to their pain. Currently, diagnostic laparoscopy (minimally invasive surgery) is the only effective means by which to properly diagnose adhesions. What can you do when the treatment you’re undergoing is not yielding results? Be proactive in your own care! Learn as much as you can about your disease and network with others who share your pain. Don’t settle for a first, second, or even third opinion if you’re dissatisfied with your treatment. There is hope! Although the journey to a solution may not be an easy one, sometimes taking the route around an obstacle can be even more effective than trying to climb over it.
Adhesions – Hope For Those Who Suffer From Adhesion Related DisorderAdhesion sufferers have felt the spin. Medical spin, that is. Like the child who waits for the parent to take him off the merry go round (I’ve had enough fun, thank you) the person who suffers from adhesions often feels trapped in a vicious cycle of pain, repeated medical tests, yet no answers. Most adhesion sufferers see doctor after doctor, with each one giving the ill patient the proverbial medical whirl. Time passes, pain continues, yet most sufferers feel compelled to seek out another doctor, i.e.: jump on a new carousel. Sick, (often in terrible pain) they muster up the strength and continue the search for that special doctor…hopes held high that he or she has a new manner (EUREKA!) in which to rotate that infuriating medical platform. For some strange reason, the optimistic person who suffers…and suffers…and suffers…holds high expectation that somewhere along the way there will be that one-in-a-million doctor who will turn them in the right direction; the doctor who will know how to lead them out of their life of misery by doing what no other doctor has done. Unfortunately, many adhesion sufferers learn the hard way that though many doctors will have the opportunity to grab the wheel and throw them for a spin, they often continue going the same direction they have been a thousand times before! Is the sufferer simply daft? After all, Albert Einstein said: the definition of insanity is doing the same thing over and over again while expecting a different result. However, the person who suffers in illness certainly has no desire to ride the medical merry-go-round; rather they realize they have one of two choices: 1. Give up and succumb to a life of pain and misery. 2. Cling to hope while desperately grasping for that elusive medical thread that surely hangs somewhere across the vast expanse of the universe! For the adhesion sufferer, education is the key factor to understanding the complexity of this horrid illness. Many physicians admit their defeat to this illness, while others deny that adhesions cause pain. (OUCH!) (Of course, those who deny that adhesions cause pain obviously do not have their internal organs stuck together.) The majority-yes majority-of physicians will never mention the possibility of adhesions when the patient presents with painful abdominal or pelvic complaints. Rather, most adhesion sufferers walk away with suggestions of IBS, Crohn’s disease, depression, spastic colon, or… This medical spin of the ill is why most adhesion sufferers search 7-10 years for an answer to their pain. And, many, many patients diagnose themselves. Which leaves us with one question: Is there a doctor in the house?
Adhesion Related Disorder (ARD)Adhesions. Many people have never heard the word, yet may be suffering from the many disorders they cause. Adhesions, otherwise known as scar tissue, are fibrous bands that form at the site of injury. Since surgery is injury (trauma) to the body, adhesions form at the site of incision. Though adhesions can cause no problems for some post surgery patients, other patients may find themselves experiencing excruciating, often debilitating pain due to adhesions that have not only formed at the site of incision, but have continued to develop, sometimes years after surgery, causing internal organs to become fused together. Adhesions can cause loss of flexibility by preventing the intended and natural fluid movement of internal organs. The scar tissue pulls the organs together and away from their normal positions. When the intestines become involved, the victim of this disorder may experience abdominal pain, nausea, and vomiting. Adhesions are the number one cause of bowel obstructions, as the scar tissue kinks or twists around the bowel, preventing the flow of content through the digestive tract. When a bowel obstruction occurs, pain (often excruciating), nausea and vomiting will likely follow as the content moves its way back up, unable to flow freely through the constricted bowel. A bowel obstruction is a medical emergency which could result in death without medical intervention. Unfortunately, many people suffer from this painful disorder for years on end, not knowing what is truly going on inside their bodies. Since surgery is the #1 cause of adhesions, doctors (and surgeons) are reluctant to discuss this all- too- common ailment. Moreover, in cases of bowel involvement, doctors may refer to constricted bowel tissue as „narrowed bowel“ or „narrowing of the bowel,“ rather than using the medical term adhesions or scar tissue. Improper medical terminology can leave the victim uninformed as to the true cause of the „narrowed bowel.“ Unfortunately, misinformation can leave some victims of adhesion related disorder with the belief that their painful condition is simply their sad lot in life.
1. Endometriosis is a condition where tissue similar to the tissue which lines the uterus is found elsewhere in the body. This misplaced tissue–endometrium–develops into growths or lesions that can be found in the abdomen and (or) pelvic cavity. The tissue responds to the menstrual cycle in the same way that the tissue in the uterine lining does: by building up, breaking down and shedding. Though menstrual blood flows from the uterus and out of the body via the vagina, blood and tissue from endometrial growths have no way to leave the body. The study of endometriosis often produces a common theme: Endo causes pain and endo causes adhesions (scar tissue). What is not found (or is rarely found) is this: Adhesions cause pain and endo causes adhesions. Though there would be no argument that misplaced tissue in the body that is reacting in the same manner as one’s monthly cycle could certainly cause pain, there seems to be little emphasis and explanation given to the overall debilitating impact that adhesion formation can play in the illness of a woman who has been labeled as an „endometriosis sufferer.“ Let’s consider what we do know: when we study endometriosis, we learn that when misplaced endometrial tissue become trapped, the surrounding tissues become inflamed and irritated. We often read about scar tissue (adhesions) forming at the site of these misplaced (implanted) tissues. However, more often than not, the information about the scar tissue (adhesions) often ends as quickly as it is mentioned. As the reader continues on, the emphasis returns back to the disease of endometriosis and how the disease can progress to severe pain, scar tissue, infertility, bowel problems, nausea, vomiting, intestinal pain, back pain, etc. But wait a minute. Adhesions, are bands of scar tissue, known to cause: severe pain, infertility, bowel problems, nausea, vomiting, intestinal pain, back pain, etc. Adhesions form as a result of inflammation or injury, and can cause organs to become fused together. This particular condition: adhesions–an illness that is often in and of itself–is rarely a topic of discussion among doctors to their patient. Endometriosis, on the other hand, an illness that has gripped the lives of 89 million women worldwide, is readily discussed as a topic of disease and pain from doctor to patient. Now, we must wonder: how many people worldwide are suffering from adhesions? Who has the magic number? Is there a magic number? I haven’t found one. It seems no one is tallying the poor souls who suffer from adhesions. This must mean that adhesions are not prevalent; not worth the census. However, if this is an illness that is shrouded in silence–and it is–who is to say the demographic impact of adhesions? Do we negate the fact that the disease known as „endometriosis“ gives way to inflammation and that inflammation gives way to adhesion formation? Do we negate the fact that adhesion formation can cause the the internal organs to fuse together, leading to a painful condition known as adhesion related disorder? In addition, do we negate the fact that 93% of patients who undergo major abdominal or pelvic surgery will develop adhesions, with over 50% of those people finding themselves facing a problematic condition known as adhesion related disorder? Do we negate the fact that c-sections are trauma to the body, as is any surgery, and that the body responds to this trauma by adhesion formation at the site of injury? Do we negate the fact that any inflammatory condition within the body can create favorable conditions for the formation of adhesions? (Endometriosis, ovarian cysts, PCOS, PID, are just some to consider). For the woman who has been told that she suffers from endometriosis, it is often difficult to find the ‚ME‘ who is caught in the middle of an illness that doctors refer to as: puzzling, perplexing, and baffling, as well as one for which they have no answer. Perhaps one piece of the puzzle that clearly fits, but many doctors fail (or refuse) to connect (or discuss), is the fact that adhesions can be a major contributor of debilitating pain and symptoms, and in some cases THE major cause of pain and symptoms in many cases that have been labeled as „endometriosis.“ Could it be that there are women who are living with a painful and debilitating condition known as ADHESIONS, yet they have been told they must live with the pain of ENDOMETRIOSIS? Each person must be her own best doctor by studying the illnesses that seem to puzzle and perplex health professionals. For once a disease is termed: puzzling, perplexing, baffling, this terminology alone can set a precedence of hopelessness in the minds of those who suffer. This hopelessness can cause many to succumb to a life of pain and suffering with the hope that one day the medical world will find an answer to the perplexing and baffling illness of endometriosis. When trying to find the ‚ME‘ in endometriosis, it behooves the sufferer to also study the illness of adhesion related disorder, as well as the impact adhesion formation can have upon the body when an inflammatory condition such as endometriosis has been determined. Note from the author: The intention of this article is not to minimize or lessen the serious illness of endometriosis. I recognize the fact that some cases of endometriosis present with little to no adhesion formation. I also recognize the fact that some women have been diagnosed with endometriosis only to later learn that they were (are) actually suffering from adhesions. This article is written to emphasize the adhesion factor that is often overlooked and perhaps never discussed between a woman and her doctor. 1. Sources: The Endometriosis Association
|

